Sonodynamic PDT - Developing Photodynamic Therapy by using different energy forms?
What is Photodynamic Therapy (PDT)?
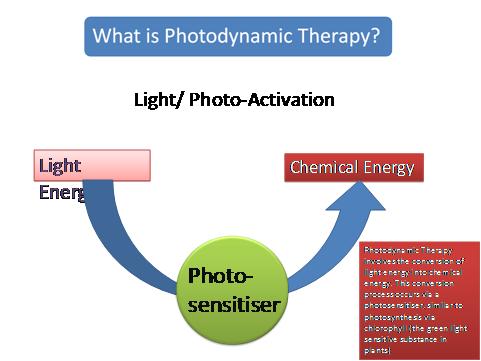
What is Photodynamic Therapy?
PDT is one of those new, ’alternative cancer therapies’ - except it has been around for over 100 years! PDT traditionally uses an active agent, which passes around the body and locks onto cancer cells. The agent is then activated by light of a specific frequency to produce singlet oxygen which kills the cancer cells.
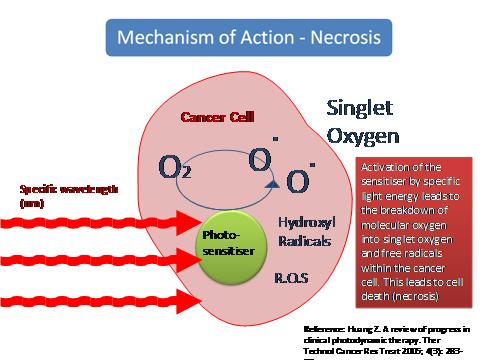
The principle behind it is that the singlet oxygen kills cancer cells - Otto Warburg won a Nobel Prize for this discovery in 1932. But singlet oxygen is even more dangerous than that and can in theory kill any cell in which to which it is attached. Thus targeting cancer cells needs to be as accurate as possible.
The problems have always been two-fold:
Firstly, can there be an agent which can achieve this tight targeting and exclusively lock onto cancer cells? If it doesnt then obviously the whole treatment might miss a few cancer cells, which would divide and take you back to square one in no time at all. Or worse, you dont want the singlet oxygen killing healthy cells around the cancer tumour either, because it has not been specific enough to just lock onto cancer cells. Hitherto, with some of the chemical agents approved for use in PDT, twenty five per cent of the cells killed were actually healthy.
Secondly, it is easy to see how Aloe Vera, or mangostein, or similar local cancer remedies might have been used by ancient civilisations to treat superficial skin conditions when exposed to sunlight. But how do you deliver light deep inside the body to treat a breast or lung tumour?
Photodynamic Therapy Developments
Fortunately, in the last 20 years there have been significant developments with lasers and other delivery systems for energy of the specific frequencies needed to activate the newer agents.
So that takes us back to the all-important agent used. Agents such as Photofrin, a product from pigs blood, have been approved and used with limited success. A few years ago, along came the Russians. They studied algae, chlorella and spirulina because the chlorophyll molecule (the molecule that makes plants green) resembles the haemoglobin molecule except the former has magnesium at its centre whilst the latter has iron. This similarity allows the chlorophyll molecule to pass reasonably freely within the blood system. And as most schoolboys will be able to tell you, shine light onto chlorophyll and you produce oxygen, the enemy of the cancer cell.
We have much more on this web site about PDT and important developments and treatments.
Sonodynamic Photodynamic Therapy (SPDT)
One of the issues with PDT is trying to develop a system that can tackle deep-seated cancers. Scientists are exploring modern light forms including lasers and ultrasound to activate the agent. Using ultrasound is termed Sonodynamic PDT. It is a version of the ’alternative cancer therapy’ of PDT. And it is similarly non-invasive.
Equally scientists are looking for agents that can work deeper and all over the body and ’green’ agents based on chlorophyll from algae are also much studied.
Several orthodox and private clinics are looking at both these features. One, the private UK Dove Clinic, have been using Sonodynamic Photodynamic Therapy on a range of late-stage cancers for 5 years. They state that It is a non-invasive, well-tolerated and clinically effective, targeted cancer treatment capable of killing cancer cells on both the surface of the body and in deep tissue. In a somewhat surprising comment given the orthodox centres in the USA who have been looking into SDRT, the NHS has warned in December 2012, that ’Doctors promoting SDRT are ’misguided or fraudulent’. A little harsh, one might think! However, despite case histories, SDRT has no clinical trials to support it.
The Dove did publish a paper in the journal Current Drug Research, covering 115 patients treated over the last 5 years. This showed encouraging results, across a range of different cancer diagnoses. Some examples in this paper included the following:
SPDT Treatment Process
The treatment process is separated into a number of clearly defined steps, and we quote directly from the paper by the Dove:
Step 1 - Administration of a Light and Ultrasound Sensitive Medicine
Sonodynamic Photodynamic Therapy (SPDT) utilises a new light and ultrasound sensitive medicine, (commonly called the agent) Sonnelux-1 that is administered under the tongue. Sonnelux-1 is developed from chlorophyll, the green coloured light-sensitive molecule in plants that allows photosynthesis. Uniquely, it is preferentially taken up by cancer cells rather than healthy cells and is safe and non-toxic.
Step 2 - Activation Using Light (Photodynamic Therapy)
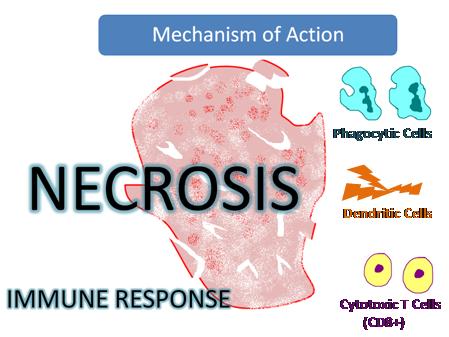
Photodynamic Therapy involves the conversion of light energy into chemical energy by using the characteristics of the photosensitive medicine (agent). Light energy of a specific wavelength is absorbed by the photosensitiser causing an excited electron state capable of transferring energy to Oxygen (O2) within the cancer cell. This breaks down O2 into singlet oxygen and other reactive oxygen species, inducing necrosis and cancer cell death.
Step 3 - Activation Using Ultrasound (Sonodynamic Therapy)
Ultrasound is used widely in diagnostic imaging for its excellent tissue penetration and safety profile. Ultrasound has the capacity to activate the photosensitiser within deep tumour tissue that is otherwise inaccessible to light. SPDT uses low-intensity ultrasound applied via a probe placed on the skin over known tumour sites and creates further singlet oxygen production and cancer cell membrane changes (sonoporation) leading to cancer cell death (necrosis) and immune activation.
What is Sonodynamic/Photodynamic Therapy (SPDT)?
Previous Research
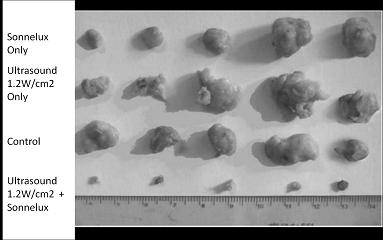
Animal cancer studies have been performed using Sonnelux SPDT. This diagram shows tumours excised after Sonnelux administration only (top line), ultrasound only (second line) and a control group with no active treatment. There is no significant difference when applied individually compared to the no treatment control group. However, when BOTH Sonnelux and then ultrasound are applied together (bottom line) a significant reduction in tumour mass occurs with cancer cell death evident.
Ref: Wang et al Integr Cancer Ther 2008; 7: 96-102
Clinical Use

Sonnelux 1 is administered slowly over 2-5 hours under the tongue. This provides sustained low plasma concentration and accumulation of the agent in the tumour tissue. 48 hours after the administration of the agent the patient is exposed to a light bed containing 48 panels of Light Emitting Diodes emitting a combination of visible and infrared light at the frequencies 660 nm and 940 nm.
No photosensitivity from normal light, artificial or natural, has been noted but as a precaution patients are advised not to stay in direct sunlight for periods over half an hour for one week following Sonnelux -1 administration. Light bed exposure time varies, with shorter exposure duration in cases with large tumour load, to try and reduce the inflammatory response which occurs following tumour cell necrosis.
Ultrasound is then applied at 1 watt/cm2 and a frequency of 1Mhz at sites of known malignant disease with time varied on a case-by-case basis depending on tumour load.
Light and ultrasound activation is repeated on three consecutive days and the same process of Sonnelux 1 administration followed by light and ultrasound exposure is repeated after one week to complete the treatment cycle.
Ozone Autohaemotherapy is administered immediately before light bed exposure, aiming to further increase singlet oxygen levels (p02) at the tumour site. Clinically, this has been observed as significantly increased tumour cytotoxic effect of SPDT, and we have an objective study showing that this use of ozone normalises the p02 levels in tumour tissue.
A course of oral Dexamethasone is administered to tumour patients depending on tumour type, background, physical status and total tumour volume along with the SPDT protocol.
RESULTS
Case Reports
Case 1. Brain tumour Ependymoma
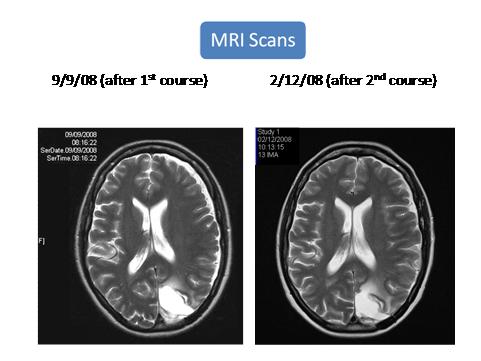
This 50 year old female patient first came to The Dove in April 2008, with a massive Ependymoma first diagnosed in April 2003. At first consultation her clinical state was poor, with a predicted median survival time of 6 months. She had previously undergone surgical de-bulking and whole brain radiotherapy. She had refused management with Temozolamide. Sonnelux-1 protocol was performed in April 2008. Dexamethasone was prescribed for the treatment course (2mg twice a day). A month after treatment she felt well enough to go on a 2 month holiday abroad. She has remained relatively symptom free. A further course of sonnelux-1 protocol was performed in October 2008. Repeat CT scans in December 2008 showed that the tumour had decreased in size.
Case 2 - non-small cell lung cancer, possibly secondary breast cancer
This 82 year old patient first came to The Dove in June 2006. She had a previous history of right-sided breast cancer in 2002 treated by lumpectomy with no chemotherapy or radiotherapy. This tumour was oestrogen and progesterone receptor negative. She used to smoke heavily until 30 years ago.
She had been complaining since December 2005 of a persistent troublesome cough and recurrent chest infections. A chest X ray was performed in January 2006 which revealed a 1.8cm soft tissue density in the left upper lobe. She was subsequently referred urgently for further investigation and was given the diagnosis of a breast cancer secondary or a non-small cell lung cancer primary. TB testing was performed for completeness, and was negative. The respiratory physicians felt that biopsy was not possible due to the location of the tumour and the associated bleeding risk. Subsequently she underwent a follow up chest X ray which revealed the mass had doubled in size between January and May 2006. She underwent a PET scan in May 2006 which did not show any other focal changes. She was recommended to have a fractionated course of radiotherapy, but turned this down. She decided to do SPDT. We carried out this treatment on her in July 2006. Her chronic cough cleared up after the SPDT and she stopped having regular chest infections. She has undergone regular chest X rays since the SPDT which show that the previously enlarging mass is stable and has remained so. She remains symptom free.
Case 3 metastatic non-small cell lung cancer
This 58 year old female first came to see The Dove in May 2007. She had been complaining of a persistent cough over the previous 10 months with a 40 pack-year smoking history. After recurrent courses of antibiotics she had a chest X ray which revealed a 6cm left upper lobe mass. She was diagnosed following a scan and her biopsy as having a non-small cell lung cancer in the left lung. Also CT the scan showed a metastasis on the right adrenal. On clinical examination at the time of presentation she had no breath sounds detectable in the left lung. She had been given a prognosis of weeks, and referred to palliative care nurses. We treated her with SPDT in July 2007. Her cough cleared up and breath sounds were detectable again in the lung approximately 2 months after the SPDT. She requested a further scan at that time but due to there being no conventional active treatment this request was refused. She developed a cough again towards the end of 2007, also air entry was again reduced on the left lung at that time and she was experiencing marked right loin pain from the adrenal metastasis. We carried out another course of SPDT on her at the end of 2007. Her cough cleared up again and clinically air entry returned to her left lung. This time she had some pain in the left chest and tiredness associated with the SPDT although this was controlled symptomatically and resolved over 4-6 weeks. The pain she had experienced in the right loin fully settled post SPDT and has not returned. She has had a follow-up scan in the Autumn of 2009, following developing visual symptoms, and this showed a solitary brain metastasis. It also showed that the lung primary was stable from previous imaging and that the previous pleural effusion had fully resolved. Also, there was a significant reduction in the adrenal metastasis. She has recently completed whole-brain radiotherapy, and is currently clinically stable.
This case shows sustained symptomatic improvement following SPDT, stable lung disease and improved adrenal pathology on follow up imaging 2 years after diagnosis.
Case 4 Metastatic squamous cell carcinoma of the anus.
This 56 year old female patient was diagnosed with squamous cell carcinoma of the anus in April 2006. She underwent chemotherapy and radiotherapy with an excellent response and at that time she refused an abdominal/perineal resection. No evidence of recurrent local or distant metastatic disease was seen on two follow up scans.
In August 2007 a CT scan revealed a 16 mm liver lesion, this increased to 3 cm in October 2007. Radiotherapy was not offered due to her previous treatment and she was offered a partial hepatectomy with neoadjuvant chemotherapy. She turned
down the neoadjuvant chemotherapy and decided to have a course of SPDT which she did in October 2007. She went on to have a partial hepatectomy, and histology confirmed extensive tumour cell necrosis and showed 3 tumours in the resected section, each tumour having extensive central necrosis. She only had a small number of tumour cells in each secondary, the vast majority consisted of necrotic tissue. She remains well and disease free.
Case 5 Metastatic breast cancer
This 66 year old female patient came to see The Dove in August 2007. She had a right sided breast cancer diagnosed in 2002 followed by a right mastectomy followed by chemotherapy and radiotherapy. This was oestrogen receptor positive and node positive. She was offered chemotherapy in 2007, which she refused. When she came to see us she had widespread tumour in both sides of the chest, with glands in the right supraclavicular fossa. CT and bone scan at that time was clear. She decided to do SPDT. We did this under Dexamethasone cover, but she still got a marked inflammatory response to the area treated with ultrasound. This took some 3 months to settle down. All tumour cleared from the treated area of the chest, but she eventally developed some recurrence above and below the ultrasound treated area. Of interest was the clearly observable fact that no tumour recurred in the ultrasound treated area. The delineation between the ultrasound treated areas and the areas where recurrence was occurring was most impressive in this patient, and almost had the precision of a straight-line division.
This patient had further SPDT in 2008.
Unfortunately she developed bone secondaries and died in May 2009.
Case 6 Metastatic breast cancer
This 47 year old came to see The Dove in 2008. She had had a right sided breast cancer in November 2004 for which she had a mastectomy, the tumour was oestrogen receptor positive. She refused radiotherapy, chemotherapy and Tamoxifen. She had a local recurrence along the scar 9 months after the mastectomy and spread into the neck lymphatics. She agreed at that time (2006) to go on Tamoxifen. In spite of the Tamoxifen the tumour continued to spread. We saw her in August 2008 and she had several involved lymph nodes in the right and left supraclavicular fossae and widespread tumour across the right side of the chest, clearly extending deeply, together with a fungating lesion in the centre of the chest. We carried out SPDT on her in September 2008. She developed a marked inflammatory response which as in the previous case lasted for approximately 3 months. This resulted in complete resolution of the tumour in the treated area which was replaced by fibrous tissue. We followed this with another one week course of SPDT in January 2009. Again, a similar response occurred.
She has recently developed a recurrence, again as in the previous case, with an almost straight-line division between the ultrasound treated area and the areas above and below it in which the recurrences are currently situated. We are currently treating her further with SPDT.
PDT CONCLUSIONS
PDT has long been thought to be a cancer treatment of huge potential. If only.
If only one could find an agent that could lock into cancer cells more specifically.
If only one could find a way of energising that agent for deep tissue cancers.
New developments are still needed to turn this ’potential’ into reality. Mike Richards, the former UK cancer Tsar was looking at investing in PDT research exploring both new agents and new energy forms. However he has stepped down from the post.
There seems little doubt that SPDT warrants further investigation as a non-invasive, well-tolerated and highly targeted cancer treatment capable of killing cancer cells at both superficial and deep malignant sites.
It may have taken over a hundred years, but just maybe PDT is at last coming of age.
However, it’s a question of wait and see, because PDT in any form still doesn’t seem to be anywhere near the fully finished article as yet, even if it can be of some benefit.