
Doing the Light Fantastic! Killing cancer with light and secret agents.
This article looks at the development of the non-invasive, alternative cancer treatment, Photodynamic Therapy (PDT) and how chemical, or plant, agents are used to lock on to cancer cells. Then light of a specific frequency energises these agents and realeases ’singlet oxygen’. And this kills the cancer cell. It’s a 100-year old theory, full of potential that just may work someday to kill all the cancer cells in a person’s body.
Originally published in icon Issue3 2006
Chemotherapy, drugs and smart bombs
Historically, chemotherapy had its critics because the chemotherapy agents were too general. They caused disruption in the copying process of cells and so would most disrupt rapidly dividing cells, which of course included cancer cells.
Unfortunately, a lot of other cells in the body divide during the chemotherapy period. Result: Many of the bad cells were killed off, along with too many good cells as well. Worse, there was no guarantee the chemical agent had destroyed all the cancer cells rather than most. Leave just one healthy cancer cell behind and the potential is there for multiple division and reoccurrence of cancer.
Nowadays scientists are developing smart chemical agents, the sort that targets some physical property unique to a cancer cell for example its unique enzymes. After all, if the American military can target a single building in a whole city with a cruise missile, why cant cancer scientists target unique cancer cells amidst a body of otherwise healthy cells? And so we increasingly see much more targeted, more cancer specific chemotherapy agents like Herceptin and Glidel. Plus a future promising more pre-tests to discover the patients likely success with the chemotherapy agent before it is used and even genome studies followed by tests on individuals to discover susceptibility to certain cancers in the first place, and thus the most appropriate, and targeted (smart) drugs to use if the need arises.
Go to: A short overview of the latest developments in PDT
However, even with the smart anti-cancer bombs two problems remain. Firstly, there are side effects (worryingly more than you would expect from this new breed of smart drugs, supposedly designed to only target the unique cancer biochemistry). Secondly, there is the ability of the cancer cells to adapt and become resistant to the chemo agent over time. Cancer cells can be smart too. These may be just two reasons why only recently the prestigious MD Anderson Cancer Center in Houston stated that all the exciting developments in cancer treatment were in areas other than traditional chemotherapy.
The crucial issues facing oncologists the world over are thus highlighted:
Can we develop agents that specifically target and kill cancer cells........
leaving healthy cells untouched
that are natural, and non-toxic to the healthy mass of the human body and
ideally kill all the rogue cells, or allow for repeated treatment as needed?
Not too much to ask, is it?! Phew!
Light relief - non-invasive ’alternative’ cancer treatment PDT
And so we come to PDT: Photodynamic Therapy. PDT is a treatment that historically has used a chemical agent (or drug as officially defined by the US National Cancer Institute) called a photosensitising agent that selectively attaches to cancer cells. When light of a certain wavelength or frequency was shone on the agent, it excited the agents atoms encouraging them to offload electrons to any oxygen molecules in the localised vicinity. These then became singlet oxygen, highly unstable free radicals.
In turn these oxidised any molecule they came into contact with. And since the original agent was specifically selected and developed so that by now it was either attached to, or inside, the cancer cell, the host was destroyed. At least, that was the principle. (1, 2, 3, 4)
Professor Hopper; University College, London Hospital, NHS Trust stated in The Lancet (December 2000): PDT is a minimally invasive treatment with great promise in malignant disease. It can be applied before, or after, chemotherapy,
ionising radiation, or surgery, without compromising these treatments or being compromised itself. Unlike radiotherapy and surgery, it can be repeated many times at the same site. Response rates and the durability of response with PDT are as good as, or better than, those with standard locoregional treatments. Furthermore there is less morbidity and better functional and cosmetic outcome.
So far, so good. Were on our way!
Light years of PDT development
Lest you have never heard of PDT and/or think it is some sort of new and probably flaky cancer treatment, please be clear.
The technology is supported by over 100 years of research and development; there have been over 4,000 scientific reviews and articles and there are currently several hundreds of universities and top cancer clinics from New York to Russia seeking to develop and improve this treatment. (Try the Internet site www.medline.com and type in PDT, for example). A quick search on the internet will reveal over 1,400,000 references.
The Americans do try to claim that somehow their National Cancer Institute invented PDT at the Roswell Laboratories in the 1970s but this is just not true; indeed Neils Finsen won a Nobel Prize in 1903 for using light treatment to cure Iupus.
In 1904 the first recorded cure of a cancer took place in Germany, a basal cell carcinoma of the lip.
However the over-excitement of the pharmaceutical and medical establishments for chemotherapy saw PDT put on the back burner until the mid-1970s when a doctor in Buffalo, NY developed a chemical agent and used it to treat cancer. The original agent was developed by Dr Thomas Doherty and named as Photofrin. (Photofrin is a registered, patented agent). This particular agent used haemoglobin molecules and was originally derived from blood, usually pigs blood.
To date the US Food and Drug Administration (FDA) has approved Photofrin (more correctly Porfimer Sodium), for use in PDT to treat or relieve the symptoms of oesophageal cancer and non-small cell lung cancer. (5) Since this was virtually the only agent used in the last part of the twentieth century, it probably explains the US claim to have invented PDT. (6)
The Roswell Park Cancer Institute now only claim to have developed PDT. Their web site (http://www.roswellpark.org) states that A non-toxic drug called Photofrin is injected intravenously. Both normal and malignant cells absorb the drug. However, two to three days later, Photofrin concentrates in the cancer cells and is reduced in the normal cells that are near many cancers. Non-thermal (without heat) red-light, which is generated by laser, is applied to the tumour. This light activates the Photofrin, causing an almost immediate destruction of the tumour cells.
PDT - Optical illusion?
PDT using Photofrin does appear to shrink or destroy tumours. (1, 2, 3, 4) It can also destroy the blood vessels supplying the tumour and, in some cases, actually stimulate the immune system (11). But, as with chemotherapy, the treatment is only as good as the chemical agent used. Photofrin is a porphrin and porphrins do selectively attach to cancer cells. However, (in some cases up to the 25 per cent level), the agent also attaches to healthy cells and all (good and bad) are killed when the localised area is sensitised by light of a certain frequency. The quest over the last thirty years has been to find better, more selective agents.
Another limitation historically, has been the need to have the cancer in a position where light could get at it and activate the agent accumulated in the cancer cells. So, for example, work with brain tumours was confined to moments when the skull had been opened up (10).
However the limitations of this direct action meant that cancer cells not exposed to the light frequency escaped. Thus early procedures where the norm was to treat tumours that were seen, often omitted dealing with any secondaries or colonies of cancer cells that had not been spotted in other areas of the body.
Early agents were also slow, both to reach cancer cells and then to clear out of the body afterwards. Photofrin can take two to four days to successfully attach to the cancer cells, and up to 50 days to clear the body. Another agent currently used in the UK, Phoscan (or Foscan), has similar problems. Roswell Park warn patients to avoid direct sunlight and strong artificial lights, like spotlights for a period of 4-6 weeks after the initial injection. Even hairdryers are to be avoided, as the heat can activate the drug retained in the scalp.
The US National Cancer Institute officially warn that porfimer sodium makes the skin and eyes (you must wear dark glasses) sensitive to light for up to six weeks and Cancerbackup (now MacMillan) even talks about the need to use low powered lighting in the home.
PDT - Making light work
PDT is improving all the time and the work is gathering pace because the agents and the technology are both improving. For example, the light delivery system can now involve lasers, even directed through fibre optic cables, using an endoscope (as in the case of oesophageal cancer). Light emitting diodes (LEDs) may be used on more superficial cancers such as skin cancers. You can easily trawl the Internet and find many clinics in the USA that use PDT. The crucial issue in the USA is FDA approval of the photodynamic agent. The FDA tend to prefer single agents rather than complex mixes.
Roswell Park lists the following cancers as treatable:
Early endobronchial non-small cell lung cancer
Other endobronchial lung tumours.
Advanced, partially or totally, obstructing cancer of the oesophagus.
Other lung cancers, including mesothelioma (post tumour removal and during surgery)
Barretts oesophagus in conjunction with high-grade dysplasia
Skin cancers (one or two treatments may be necessary)
Breast cancers (local recurrences following mastectomy)
Colorectal tumours (PDT used to kill cells remaining after surgery)
Gynaecological malignancies (vagina, vulva and cervix)
However, much work is going on in the world of PDT. Elsewhere it is being used to treat brain (11), breast (8) and pancreatic cancers (12). Here are just a few examples.
Roswell Park themselves now use ALA (5-aminolevulinic acid) as a topical agent for skin cancers, and a new agent called Photochlor is increasingly replacing Photofrin. Both avoid the long lasting light-sensitivity of Photofrin.
The Mayo Clinic (http://www.mayoclinic.org) are also investigating new agents and list virtually all the cancers of Roswell Park as treatable, plus gastric cancer. Their list includes the treatment of macular degeneration where they claim PDT destroys abnormal blood vessels too.
In 2003/4 the team at the Johann Wolfgang Goethe University in Frankfurt treated five liver cancer patients with an agent called SQN400. All had colorectal cancers that had spread to the liver; three of the five were clear of cancer three months later.
Combating low oxygen
In April 2003, icon magazine reported on a trial at the Gray Cancer Institute in Middlesex and sponsored by Cancer Research UK. The trial, reported in the journal Cancer Research, used a dye combined with plant hormones. When they shone red light on the cells with the dye, the dye shattered and provided chemicals toxic to
the cell.
Professor Peter Wardman, who led the study for Cancer Research UK, drew attention to the problem of low oxygen in the cancer cells. The problem with PDT historically was that it worked by activating localised oxygen to produce singlet
oxygen, which destroyed the cells (as we said at the start of this article). But in most tumours there are low oxygen conditions to start with, reducing the ability of the agent to work effectively. Where does it get the oxygen from? Wardmans method uses molecules of plant hormones to attack cancer cells instead. Overcoming this oxygen problem is a major challenge in cancer therapy. So far we have shown this works in dishes, but because both the dye and the plant hormone are known to be non-toxic in man, we are hopeful that we can quickly translate this treatment into clinical reality.
Interestingly the new Roswell Park agents are based on plants, using derivatives of chlorophyll.
In Russia there is much work on PDT currently. In one company, Rada Pharma, scientists and pharmacists have developed a triple ingredient agent based on algae and chlorophyll, called radachlorin. They are currently investigating it in trials (reportedly in Holland and Belgium) as the nature of the agent allows light of the infrared range to be used to sensitise the agent. This would enable the body to be harmlessly penetrated by the light and so deep-seated tumours and their metastases could be attacked. This in itself would be a major breakthrough as historically PDT could only be used on superficial cancers (skin cancer) or by methods such as fibre optics where light could be delivered to a solid tumour.
Algae, chlorophyll and PDT active agents
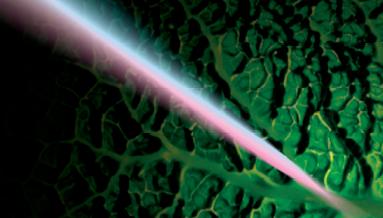 It has long been known that the chlorophyll molecule in plants resembles that of haemoglobin in animals. They are structurally similar, the main difference being an iron atom at the centre of haemoglobin, but a magnesium atom in chlorophyll.
It has long been known that the chlorophyll molecule in plants resembles that of haemoglobin in animals. They are structurally similar, the main difference being an iron atom at the centre of haemoglobin, but a magnesium atom in chlorophyll.
Both are crucial in the oxygenation process in an organism.
In plants, sunlight energises the chlorophyll causing oxygen production, a totally natural process. Thus, in theory, the use of chlorophyll and similar agents could provide their own oxygen, overcoming the problem identified by Wardman above.
Populations that consume large amounts of green plants and have lots of sunlight (for example, Mediterranean cultures, or the sun belt in the USA) get less cancers, and it is known that, along with higher vitamin D levels, longer wavelength UV plays some part in this.
Some diet therapies involving barley grass, spirulina or wheat grass in part attribute their success to the oxygenating benefits of chlorophyll.
Russian research has looked into chlorophyll, algae and bacteriochlorophyll,
the latter being a red type of chlorophyll sensitive to light in the infrared range. This is important because such infrared light can penetrate deeper into the body than the light used for such agents as Photofrin and sensitise the agent in deep seated tumours, whilst potentially hitting more rogue cells outside of the tumours solid mass.
With the Russian agent, the wait time is claimed to be only hours after intravenous infusion before light treatment can be used. And within 36 hours there is no sensitivity to light as the agent has been eliminated from the skin.
An example of things to come in PDT?
In 1998, Bill Porter was retired and living in Ireland when his wife was diagnosed with breast cancer. She did not want orthodox medical treatment because of the side-effects. Through Porter’s own work with light and lasers he became particularly interested in photodynamic therapy.
Porter managed to lay his hands on some of the Rada Pharma agent. He felt it was good, but still had problems. So he turned to yet another Irish doctor, this time also a pharmacologist, Dr. Tom Clearey, and together they specified, had made, registered and patented in the UK, their own agent Photo Flora. This of course in turn prompted the competitive wrath of, and falling out with, the Russians!! Clearey’s natural agent is also potentially a cheap, non-toxic replacement for many pharmaceutical drugs. He can expect much focus and attention on his work. There is big money at stake here.
In their view, it is probably no coincidence that the haemoglobin and chlorophyll molecules are so structurally similar given our long-term evolution as humans, nor that agricultural communities who eat more green foods and live out of doors more, develop less cancers.
Photo Flora is based on spirulina. This natural agent circulates easily in the blood system, without toxic effect, because of its similarity to haemoglobin.
The cancer cell, which produces its energy without oxygen in a fermentation process, is acidic and negatively charged. Because the energy process is less efficient than that of a normal cell, and because cancer cells divide so rapidly, a large amount of fuel is required. In a cancer cell, this fuel is glucose.
The success of Photo Flora, according to Clearey is that it acts like glucose and so gains easy entry into the cancer cells.
Glucose is normally carried across cell membranes by lipoproteins found in the blood. The agent is also carried this way.
But two other factors make it stick uniquely inside a cancer cell. First, normal cells are slightly alkaline, but by contrast the acidity in a cancer cell disengages the agent from the lipoprotein. Second, the agent has two positive charged areas and thus energetically binds to the negatively charged elements in the unique power stations of the cancer cell.
Meanwhile, the risk of binding to healthy cells falls from about 25 per cent (Photofrin) to less than 3 per cent, so Clearey claimed to me, because this new agent specifically avoids healthy cells that are alkaline and not negatively charged. So the very structure and properties of the cancer cell cause the agent to be absorbed uniquely by them. No resistance builds up to it over time either, so repeated sessions can be used.
More remarkably, the agent has been developed and a version of Photo Flora can be taken orally, using drops under the tongue.
Patients may take the green liquid for a month or just three days depending upon the level of activity required. Then comes the photosensitising treatment, which looks like a giant sunbed! Not only is this slightly less stressful since the patient merely lies on the sunbed for a few minutes per day, but it allows build up of the agent throughout the body and early indications are that luminescence occurs releasing oxygen and killing cancer cells even before the treatment starts! In an attempt to patent and brand this unique process (and thus protect the profits no doubt) the whole system is not called PDT but instead Cytoluminescent Therapy (CLT). Now what did Shakespeare say about a rose??!
Light of the correct infrared wavelength is then shone on the body to sensitise the agent. But unlike traditional PDT, the effect is not localised as the light wavelength penetrates deeply; the effects are thus more systemic, throughout the body. In this event, CLT has the potential to kill all cancer cells in the body, not just the targeted tumour in the original Photofrin example.
A further bonus claimed is that the cytoxic effects of the agent and the CLT tend to cause coagulation in the blood vessels that feed the tumour, cutting off its supply of nourishment.
And finally, it would seem that although the death of the cancer cell occurs from within, the initial breakdown of the tumour releases inactive cancer cells into the bloodstream that are mopped up by the immune system. This stimulates the immune system to recognise a better level of rogue cells everywhere. This mirrors the US NCI and Roswell findings that PDT does stimulate the immune response.
At this point I should stress that this CLT detail is just an example of work taking place at a number of research centres (orthodox and private) in the world. We are not advocating this particular treatment. Indeed Bill Porter subsequently found himself discredited in Ireland.
PDT - the potential for a non-toxic cancer cure
Photodynamic Therapy is a treatment approved for use in cancer in the USA, Britain and countries worldwide. There is hard scientific evidence on it and Clinical Trials, although no fully randomised, placebo controlled phase III Clinical Trial. This will come however.
PDT is, however, only as good as the photosensitive agent, which in turn determines the frequency of the light that can be used and thus the depth of penetration in the body and the pick up of cancer cells outside of the solid tumours.
Despite over 100 years of work already, PDT is probably only in its teenage years. We are not yet at the finished article stage. But work is accelerating, in the USA, in Russia and in various other countries including the UK to develop agents and light delivery systems. Clearly this work is worthwhile. The potential is there for a natural, non-toxic and relatively cheap way of killing cancer cells. Whilst we cannot vouch for the success of the likes of Photofrin, Phoscan (Foscan), chlorophyll agents or Cytoluminescent Therapy, we applaud the scientists trying to take this work to the next level.
PDT will hopefully, one day, become the ultimate smart bomb. Non-toxic to healthy cells, highly effective against cancer cells and simple and cheap to administer. We may not be far away from that day.
References
1. Vrouenraets MB, Visser GWM, Snow GB, van Dongen GAMS. Basic principles, applications in oncology and improved selectivity of photodynamic therapy. Anticancer Research 2003;23:505522.
2. Dolmans DEJGJ, Fukumura D, Jain RK. Photodynamic therapy for cancer. Nature Reviews Cancer 2003;3(5):380387.
3. Dougherty TJ, Gomer CJ, Henderson BW, et al. Photodynamic therapy. Journal of the National Cancer Institute 1998;90(12):889905.
4. Wilson BC. Photodynamic therapy for cancer: Principles. Canadian Journal of Gastroenterology 2002;16(6):393396.
5. U.S. Food and Drug Administration (December 2003). Approved claims for palliative line therapy. Retrieved December 29, 2003, from: http://www.accessdata.fda.gov/scripts/cder/onctools/linelist.cfm?line=Palliative
6. US FDA (August 2003) FDA approves photofrin to treat cancerous lesions in Barretts oesophagus. Retrieved Dec 29, 2003 from http://www.fda.gov/bbs/topics/ANSWERS/2003/ANSO1246-html
7. PDT, a clinical reality in the treatment of cancer. Lancet Oncology, Dec 1, 2001; 1:212-9.
8. PDT for locoregional breast cancer recurrences. Wyss et al; Int J Cancer, Sept 1, 2001; 93 (5) 720-4.
9. PDT for lung cancer: state of the art. Okuna & Kato; Nippon Geka; Feb 1 2002; 103(2), 258-62.
10. PDT: a novel treatment for primary brain malignancy. J. Neurosci Nurs, Dec 1, 2001: 33(6): 296-300.
11. The immunological consequences of PDT. Immunobiology, Vol 207, Number 2, March 2003 pp 105-113, van Duijnhoven et al.
12. Infrared Laser Activation of Indocyanine Green inhibits growth in Human Pancreatic Cancer. Tseng et al, Pancreas, October 1st 2003; 27(3):E42-45
