FIRST CLICK HERE AND READ OUR OVERVIEW
Originally published in Issue 1 2005 icon
The Secret Weapon In Breast Cancer Detection?
By Madeleine Kingsley
Once upon a time, thermography was a secret weapon. Its heat-sensing ability helped the military flush out adversaries hiding by night and led missiles to their targets. People trapped in burning buildings, lost at sea or in snowdrifts, could be rescued because their body temperature showed up as thermal images. So far, so dramatic, but when the technology was released into the public domain, 1960s physicians leapt on thermography’s potential as an equally potent life-saver in the medical sphere: cancerous tissues emit more infra-red heat than healthy tissue, so here, it seemed, was a surefire way of detecting tumours.
Zeal, unfortunately, ran ahead of clinical trials, which at the time were carried out using ex-military and industrial equipment. Thermography fell out of favour for many years but good ideas find their own right time: in the past decade thermography scanning has been re-introduced and refined in tune with greater understanding of physiology and advances in computer technology. It is now routinely used in many areas of mainstream medicine (including rheumatology, neurology, pain clinics and vascular-related dysfunction). But so far it’s been most enthusiastically embraced by the holistic health world, where its value as an extra diagnostic tool for breast disease is seen as ground-breaking:

It seems to spot active pre-cancerous breast signs some six to eight years before any palpable lump appears

Thermography’s key asset is that it seems to spot active pre-cancerous breast signs some six to eight years before any palpable lump appears. This may well be in time for wise patients to alter their lifestyle and so modify their health, reversing the earliest changes. Speedy (the whole procedure is over in 15 minutes), safe (there’s no exposure to radiation) thermography is also non-invasive (so there’s no unpleasant compression and the patient sits in a small cosy room several feet from the scanner). So could thermography be the new secret weapon in the battle against breast cancer? Could it help women avoid unnecessary mammograms and reduce exposure to harmful radiation? Could it lead the way beyond screening mammography which, on its own, only detects breast disease that is already well developed enough to be seen with x-ray? We already know that thermography works for young women where mammography is contra-indicated because their breast tissue is too dense to "read". Given the sharp rise in breast cases among younger women, this simple screening system would be hot news indeed.
The picture - for young women especially - looks good, and women would naturally wish thermography to take over from mammography because it is so simple, painless and radiation free. But Dr Peter Leando, founder and Managing Director of Meditherm, the US firm producing high specificity medical thermal scanners cautions against seeing thermography as a stand-alone diagnostic miracle: "Thermography is very much an extra, not an alternative breast screening tool" he explains, "and I stress that we are not in competition with mammography or taking on the same job. Thermography works best in clinical evaluation as an adjunct to mammography and ultrasound: a study at the Ville Marie Institute in Canada found thermography to have an 83 per cent detection rate as opposed to mammography’s 84 per cent. When combined, however the two services reached 95 per cent accuracy."

The real purpose is to establish a base line - a thermal fingerprint

A thermal scan can provide additional information about the body, but it does a different job from mammogram or ultrasound which test structure and anatomy. Thermography is a test, instead, of function and physiology and its overriding purpose in specialist breast screening, says Peter "is to monitor breast physiology and track changes over time. A first study is not really designed to identify any suspicious findings (though of course any patient would immediately be referred to her physician for further clinical investigation if worrying signs did emerge). The real purpose is to establish a base line - a thermal fingerprint, if you like, of the breast physiology that is normal for that particular patient. Everyone has a vascular structure and anatomy that’s particular to them, so what we are trying to establish in every case is whether this thermal fingerprint is stable, so we re-scan after the first three months to monitor for changes that might give concern. Thereafter women are followed up annually."
All thermologists - the medical doctors trained to "read" thermal scans just as radiologists read the x-ray pictures radiographers have taken - are highly trained to look for patterns particular to various breast conditions. These may present as asymmetry - where the colour pattern differs in one breast from the other - though repeat monitoring could also evaluate this as normal for that particular woman. "Comparing right side to left, and different areas of the breast," says Peter "we are looking for temperature differentials and particularly patterns that may be suspicious. But even if they do change over time, these differences could also relate to fibrocystic changes, and thermal ’hotspots’ could simply reflect nerve irritation."
Thermography, Peter points out, is not the appropriate first-line service for any woman with known breast cancer: "Mammography is more accurate for later stage cancer or for anyone with a palpable lump, although the thermal image can help pinpoint where the cancer is most active, and therefore act as a useful guide for more targeted mammography. Thermography only enables us to look at the activity of that lump and see if it’s very vascular, indicating angiogenesis or an active blood supply "feeding" the tumour.

Thermal scanning can’t give the information a mammogram provides in terms of size, density and order of the lump

Thermal scanning can’t give the information a mammogram provides in terms of size, density and order of the lump. It doesn’t provide what pathology can; it’s purely a test of physiology. It can’t assess whether a lump is attached to the surrounding tissue, if it’s rough or smooth, filled with fluid or a denser, more solid mass. So much is involved in a diagnosis of cancer. But when thermography does produce positive findings, it justifies the more invasive tests and it does give mammography something to look for and so aids detection.
Thermography really comes into its own as preventative screening before a woman ever has a scare or is called for routine NHS mammography at 50. Although the thermal scan colour images produced look very straightforward, most women wanting the bottom line about breast health would not immediately grasp what they are seeing: "What the thermal image reflects" Peter explains, "is skin blood flow. We don’t see any organs, any depth into the body or any conducted heat from deeper structures or underlying inflammation. Any thermal patterns we do see reflect the body’s surface temperature as a neural response to whatever is going on beneath, which could be inflammation, lymph congestion or angiogenesis. Thermography works because the skin, as an organ, is totally under the control of sympathetic nerve function and thermography provides a snapshot of the body’s response on the skin surface to any disease or injury." For young women who are wisely health-conscious or, at the other end of the spectrum, concerned about the effects of lifestyle habits like smoking or drinking, thermography clearly fills a gap in the standard diagnostic screening process.
As it’s non-invasive, patients can self-refer, yet come away with a report that then becomes part of their medical record. If thermography shows cause for concern, then it’s helpful for a young woman to have something tangible to show her doctor, who might otherwise dismiss her as one of the worried well. Peter Leando says his thermography service regularly picks up patients where a slight change registers during the three months between initial scan and follow up. "Sometimes mammography is negative nonetheless, and it can take up to another year before what we first identify becomes dense enough for mammography to identify. It also takes quite a long time before biopsy can verify the finding because you have to have some physical calcification or cell growth to get a needle into."

Most women in this waiting state would rather not sit back and do
nothing

Most women in this waiting state would rather not sit back and do nothing. And those wishing to do all they can to help themselves, find their way to holistic health practitioners like Dr Shamim Daya in Harley Street. Shamim (who explains that she left general practice because "there was too much emphasis on symptomatic treatment and not enough on the root cause of the disease process") will see the situation as a wake-up call for any such patient in her care:
"I ask a lot of questions about women’s lifestyle and generally find that they urgently need to clean up their act - to cut out toxic drinks, drink more water, improve their diet, introduce an exercise programme. The aim is to minimise the toxic load that is primarily affecting the liver and creating lymph congestion. For slightly older women in the perimenopause, hormone imbalances increase stress on the body. It’s common to find that these women have a mouthful of mercury fillings, which also increases the toxic load. If the lymph congestion is pronounced, I would prescribe some herbal/homeopathic ’drainage’ remedies as well as suggesting that she drank more water and took exercise. I’d ask ’Have you done a bowel cleanse with herbal capsules recently?’ This multi-factorial approach is intended to get toxic waste out of your system as quickly as possible - that’s what the breasts are trying to tell me."
Shamim regularly sees women in their twenties who are already at risk from smoking and drinking habits that put a strain on key organs including the liver. Her message to them cuts straight to the chase: "Please don’t wait till your thirties, when you have a family and a drastic diagnosis like breast cancer is the last thing you need." She is quietly confident that indications of early breast damage can be reversed, "although in my experience thermography doesn’t pick up a problem that will go away on its own. That’s why we monitor. The importance of follow-up scanning is to check for the progress of disease or its reversal, provided my recommendations are followed. If things aren’t improving as we would hope, then it may be necessary to take a more aggressive approach to reduce the toxic load, adding in specialist infrared saunas, correcting any underlying hormonal imbalances using bio-identical (natural) hormones and carefully supervised removal of mercury fillings together with liver-supporting remedies.

We can only advise and leave the responsibility to them

"Obviously we can’t force women to change - we can only advise and leave the responsibility to them. Thermography is a great tool for giving women choices and for many it’s a great motivator for change. My resident thermographer suggested screening to her own daughter, who seemed impervious to warnings about booze and fags. Motivated by her aunt’s recent breast cancer diagnosis, this young woman came along - and was shocked enough by what she saw on screen to change her lifestyle almost overnight."
Thus far the NHS shows no sign of embracing thermography So, sadly, almost all thermographic breast screening is paid for privately: "But it’s no more expensive than a takeaway coffee a day" says Dr Daya "We charge £185 for the first scan, including a three month follow up. An annual scan is £150 thereafter." Sherrill Sellman, (one of icon’s Icons and author of Hormone Heresy) has described the thermal scanner as "the most neglected piece of apparatus for female wellbeing". Cost wise, it is relatively modest - around £20,000 would buy a local Health Authority the whole kit - camera, scanner computer, all the relevant software plus training for two technicians. You could say that thermography also has the royal seal of approval, having been used to scan the four elegant legs of the late Queen Mother’s racehorses at Lambourn, Berks! Thermal imaging is very good for pain assessment and for picking up nerve damage and muscle atrophy.
However promising, the future of thermography in two-legged health will take its time to unfold. "Medical developments are always very, very slow" says Peter. "But breast screening will hopefully progress to include more physiological assessment and a combined approach using the different techniques for optimum results and early detection." Of the 600 Meditherm scanners worldwide, about half are used predominantly in breast screening - 200 of them in the US. In the first year of thermal scanning, one in 30 women presents with positive findings across the age range from 25-75. That’s one more woman who can seek early help and thank thermography for providing an extra weapon in the war against cancer.
Examples
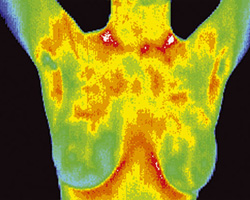
One
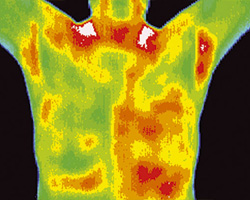
This 57 year old patient had her first scan last year. The result was worrying so we asked for an urgent report. Further investigation found that she was in need of natural hormone support; she had a mouthful of mercury fillings, metal toxicity in her liver and a sluggish lymph system round the breasts. There was no lump to feel; ultrasound and mammograms were negative.Yet something was brewing that in five years or more could have become a lump. Here we had a star patient, who was very responsive and embarked pro-actively on a six month restorative health programme. A year on you can see a classic recovery. She feels great – and relieved.
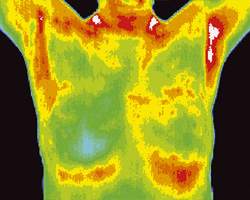
Two
This young woman in her twenties has relatively healthy looking breasts.
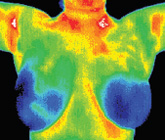
Three
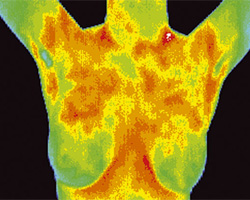
This young woman in her twenties shows lymph congestion in both breasts which seemed more marked in her three month follow up scans, prompting her to quit smoking and drinking.
The images illustrating this feature were taken with a Meditherm, Med2000 scanner.
Contact
Dr Peter Leando’s website address is: www.meditherm.com. Dr Shamim Daya BM DRCOG works from the Wholistic Medical Centre, 57 Harley St, London, W1G 8QS; Tel: 07000 388 388 Website: www.wholisticmedical.co.uk.
OTHER ARTICLES OF INTEREST
Thermal imaging