Radiotherapy, or radiation therapy, is used in nearly two-thirds of all cancer treatments, and that is more often than surgery. It’s the most cost-effective and, arguably, the least invasive of any common orthodox cancer treatments. It is claimed that hundreds of thousands of lives are saved around the world each year thanks to radiotherapy treatments. And yet it’s probably the most misunderstood and feared of cancer treatments. In this article, we asked Varian Medical Systems European Communications Director, Neil Madle, to present the facts about modern radiotherapy and how advances in imaging and software are making it more precise and effective than ever before.
For many years, radiotherapy, or radiation therapy as it is called in other countries, has been considered one of the most effective ways of defeating cancer. High energy x-rays destroy tumours by killing cancer cells which are unable to repair themselves. Healthy cells can repair themselves after exposure, provided they don’t receive too high a dose. Radiation will kill a tumour every time if sufficient dose can be delivered to the tumour itself, but oncologists are limited in the dose they can deliver because of the need to spare healthy surrounding tissue from over-exposure. This is why a typical course of radiotherapy will involve around 30 daily treatments over a period of five to six weeks.
Radiotherapy has come on leaps and bounds in recent years, with several major technological breakthroughs that have increased precision and limited ’collateral damage’. This means clinicians are able to boost doses, killing tumours more effectively, while further sparing surrounding healthy tissue. Techniques such as Intensity Modulated Radiotherapy (IMRT), Image-Guided Radiotherapy (IGRT), Stereotactic Radiosurgery (SRS) and Volumetric Modulated Arc Therapy (VMAT) are examples of this increased precision.
Today’s powerful, hyper-accurate treatments are light years away from the fearful image many people hold of radiotherapy. Today, treatments can be tailored for the individual patient and doses can be ’sculpted’ to precisely match the shape of the tumour and take account of motion during treatment.
External beam radiotherapy
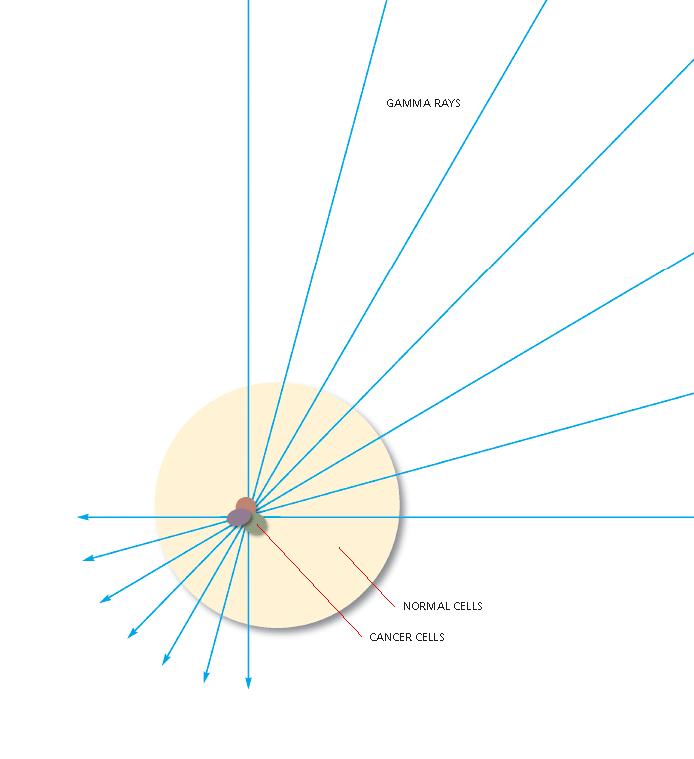
The vast majority of radiotherapy treatments involve external beam radiotherapy. With external beam radiotherapy, the patient lies in a fixed position on a treatment table. Powerful and precisely placed radiation beams are directed at the tumour using a sophisticated device called a medical linear accelerator. The accelerator rotates around the patient, delivering beams from different angles. When these beams converge on the target, their combined effect is very powerful.
The patient’s treatment will have been planned using three-dimensional diagnostic images from a CT scanner. Sophisticated software programmes use this image data to calculate the best approach for achieving the doctor’s clinical goals of concentrating dose on the tumour with minimal exposure to surrounding healthy organs and tissue. In modern treatments, all hardware and software interfaces are entirely automated and integrated.
Most hospitals accommodate patients in treatment slots of 10-20 minutes, depending on the complexity of the treatment. As we’ll see in this article, technology is now available that brings the treatment time down to just a couple of minutes, but that’s a story for later. Most modern clinical settings will schedule appointments within this standard 10-20 minute slot, providing ample time for the patient to enter the room, lie down, receive treatment and depart in comfort.
For many years, clinicians treated a wide margin around the tumour site to ensure the whole tumour received the required dose. This margin meant that doses had to be kept at a lower level to avoid damaging healthy tissue and critical organs during treatment. Tremendous efforts have been made in recent years to shrink these margins and boost doses through the use of better imaging immediately before and during treatment, and through the addition of beam-shaping accessories. The first of these advances was IMRT, which was first implemented in the late 1990s.
Intensity-modulated radiation therapy (IMRT)
IMRT is a process that enables clinicians to precisely shape the radiation beam so that it conforms to the three-dimensional shape of the targeted tumour. This is done by shaping and varying the dose as it is delivered from different angles around the patient and was made possible by the introduction of multi-leaf collimators, devices which sit in the head of the treatment machine and shape the beam to conform to the shape of the tumour.
With IMRT, doses are often delivered from multiple angles to limit the dose on entry to the patient while creating a hot spot at the tumour site. Dose can also be varied to deliver higher levels to more metabolically active parts of the tumour. The result is greater protection of surrounding healthy tissue, as well as the ability to deliver higher, more effective doses directly to the tumour.
Since its introduction, IMRT has been implemented in hundreds of clinics around the world, including several in the UK. This technique takes longer to plan and deliver than conventional 3D conformal radiotherapy treatments, which sometimes acts as a limiting factor, especially at busy public hospitals where long waiting lists are an issue.

The multi-leaf collimator shapes the beam to match the tumour
We intend to use IMRT primarily for head and neck cancer treatments, largely because of the ability to spare the parotid glands from exposure, says Alison Vinall, head of radiotherapy physics at the Norfolk and Norwich Hospital, which has been treating with IMRT for several years. One of the primary benefits of this kind of approach is to avoid what’s known as ’dry mouth’, where patients cannot produce saliva and find it hard to swallow.
In a two-year study into IMRT, the Department of Radio-Oncology at University Hospital, Zurich, treated 150 head and neck cancer patients with a form of IMRT called ’simultaneous integrated boost’ in a two-year trial. Professor Urs Luetolf, the department’s chief therapist, says, Our results showed a considerable reduction in side effects and an increase in the quality of life for patients. With treatments such as this you get a disproportional benefit if you spare 20 percent of the healthy tissue, my view is the patient feels better by 50 percent. Our treatments have shown that patients recover much more rapidly following IMRT, compared to patients treated with conventional 3D planning.
Professor Luetolf and his team have pioneered simultaneous integrated boost - a more precise way of delivering different levels of radiation dose per treatment session - for head and neck cancer treatments. This has proven particularly helpful in reducing instances of Zerostomia, a severe form of ’dry mouth’, which can result if salivary glands are over-exposed to radiation.
With radiotherapy beams focusing more tightly on the tumour thanks to IMRT, the question of motion has become increasingly important. For many years oncologists have been faced with the problem of tumours moving due to changes in the anatomy throughout the course of treatment, through natural motion inside the body, or through the breathing process. Image-guided radiotherapy, introduced in 2004, addresses that very real problem.
Image Guided Radiotherapy (IGRT)
Prior to the introduction of image-guided radiotherapy, radiation oncologists had to contend with variations in patient positioning, internal movement and respiratory motion by treating a larger margin of healthy tissue around the tumour. Because they were uncertain of the precise position of the tumour at the time of treatment, they widened the treatment field to ensure the entire tumour was treated. In essence, they used a tennis ball sized beam to treat a golf ball sized tumour. With IGRT, they can use a golf ball sized beam.
Image-guidance normally involves an imager being attached to the treatment machine, enabling near-diagnostic quality images to be taken immediately before the treatment, while the patient lies in the correct position on the couch. IGRT provides high-resolution, three-dimensional images to pinpoint tumour sites, adjust patient positioning when necessary, and complete a treatment - all within the standard treatment time slot. These capabilities take IMRT technologies one step further by raising the quality of patient care and improving efficiency.
Knowing exactly where the tumour is allows clinicians to reduce the volume of tissue irradiated, targeting only the tumour and sparing the surrounding normal tissue. Irradiating less normal tissue reduces the toxicity of radiotherapy, improving the patients quality of life. In some cases, improved targeting may make it possible to deliver higher radiation doses to the tumour and thereby increase the likelihood of local tumour control.
In short, IGRT enables doctors to locate and target tumours more accurately during treatments. This is really important because it enables us to offer more precise radiotherapy, says Dr. Andreas Rhein, senior therapist at Klinikum Memmingen in Germany. It allows us to increase the dose, particularly for our prostate patients, because we are confident that we are hitting the target and minimising the affect on surrounding healthy tissue.
Before implementing IGRT we had to use the planning CT and we brought the patient across to the planning department every three weeks or so to check positioning, says Dr. Peter Thum, head of the radiation oncology department at Kantonsspital in Lucerne, Switzerland. With this capability now on the treatment machines, we are able to do this more frequently to optimise accuracy and avoid the problem of anatomical motion when the patient is transferred from the CT scanner to the treatment machine.
Prof. Dr. Stefan Wachter, chief radiation oncologist at Klinikum Passau in Germany, adds, We wanted to be able to offer the kind of advanced treatments that a university hospital would offer. Now, in this rural environment, we can provide treatments that our patients would have had to travel to Munich to receive in the past.
He said real-time imaging using IGRT had also helped when treating patients in the thoracic region for lung cancer. We have had two patients where the cancers are influencing the anatomy of the patient by pulling up the diaphragm, he said. We have been able to re-plan the treatments for these patients based on the cone-beam CT images taken at the time of treatment, whereas this would not have been possible previously.
Image-guidance combined with IMRT has also enabled the breakthrough of fast and efficient VMAT (volumetric modulate arc therapy) treatments, the latest leap-forward in efficiency and precision.
Volumetric Modulated Arc Therapy
VMAT treatments improve dose conformity while significantly shortening treatment times. This new approach, introduced in 2008, is anything from two to eight times faster than the fastest dynamic IMRT treatments that could be delivered beforehand.
VMAT treatments deliver a precisely sculpted 3D dose distribution with a single or multiple 360-degree rotations of the medical linear accelerator gantry around the patient. Unlike IMRT where the machine stops at regular points and delivers beams from different angles to create a ’hot-spot’ on the tumour, VMAT treatments occur in continuous rotations, with sophisticated software ensuring the dose is delivered according to the treatment plan.
Machines achieve this by modifying three factors during the treatment: the speed at which the machine rotates around the patient, the shape of the treatment beam and the strength of the dose being delivered at any point.
The first person treated using a commercial linear accelerator-based VMAT system in the UK was 65-year-old father of six Graham McCormack at Clatterbridge Centre for Oncology, near Liverpool, in November 2008. Mr McCormack, who was diagnosed with prostate cancer in June, had his treatment slot reduced considerably with VMAT, with even greater savings in ’beam-on’ time. It is very exciting to be the first patient in the country to benefit from this new treatment, says Mr McCormack. I’m still employed as a sales executive within the air cargo business which keeps me very active, so the prospect of having the treatment in less time was very appealing. The treatment itself is over in minutes.
This is a major advance in radiotherapy technology that will change the way radiotherapy is planned and delivered for selected patients, says Angela Heaton, research radiographer at Clatterbridge Centre for Oncology. The benefit to patients is significant not only will they need to lie on the treatment table for considerably less time but we may also be able to treat more patients as treatment times are reduced.
According to Angela Heaton, the ’beam-on’ time for Mr McCormack was reduced from nearly four minutes with conventional IMRT to just 1 minute 10 seconds with VMAT. The total time he spent in the treatment room was reduced from over ten minutes to eight and a half minutes. In addition, the VMAT prostate plan resulted in a better dose distribution and avoidance of organs at risk, she said.
Shortly we intend to start using this for complex head & neck cancer treatments and we expect the beam-on time will be reduced from 25 minutes using IMRT to about two and a half minutes using two arcs with this system, resulting in more efficient treatments and potentially shortening waiting lists, she added.
Benefits of speed
The benefits of such fast treatments are many: the shorter time for treatment delivery not only has an economic benefit more patients can be treated within the same time but the risk of movement of the patient during treatment is also smaller, and it is of course much more comfortable for the patients. Linear accelerator manufacturers describe patients as lying on a ’couch’ during treatment but, in truth, it’s more like a table and the patients can find it uncomfortable to lie still for more than a few minutes.
It is also clear that when dose distribution is more conformal to the tumour or enables better avoidance of critical structures, a higher dose can be given, with better options for cure and lower risks of side effects. In addition, there is some radiobiological evidence from cell lines suggesting that if the dose is given in a shorter time - less than two minutes instead of 10 minutes - more tumour cells are killed.
Although it represents a major advance in radiotherapy treatment technology, VMAT is easy to implement. It requires no major process changes from the physician, physicist, dosimetrist, or therapist, as the steps for planning and delivering treatments are virtually unchanged.

VMAT involves a single or multiple rotations of the machine head around the patient, with various parameters being varied to achieve the planned dose distribution more quickly than is possible with fixed-field IMRT.
Stereotactic Radiosurgery
Whereas radiotherapy treatments take several weeks and up to 30 daily ’fractions’ to deliver the full dose, radiosurgery treatments take place in just one to five hospital visits. By using super-skinny and highly powerful beams of radiation in the same way a surgeon would use a knife, radiosurgery techniques have been used to treat tumours and lesions for a number of years. They enable oncologists to treat not just the primary disease site but to quickly and efficiently ’zap’ lesions that may develop elsewhere in the body. As with other advances, they have been made possible by far better imaging technologies.
Historically, radiosurgery began by treating targets in the brain and has now extended to targets in the spine and other extra-cranial organs. Recent studies have suggested this strategy can be more effective at killing or controlling certain types of cancer.
The clinical targets for stereotactic radiosurgery are relatively small and well defined. High-resolution 3D imaging techniques such as CT and MRI help identify and clinically define these targets and the critical structures surrounding them. Sometimes a small number of targets are treated simultaneously. As they involve a small number of fractions of radiation (hypofractionation), radiosurgical procedures are generally completed within the same week.
Dispelling myths about radiotherapy
We’ve seen how imaging advances have enabled technologies that make radiotherapy faster, more efficient and more comfortable for the patient while improving cure rates and reducing side effects. Now let’s see if we can tackle some specific misconceptions about the treatment.
The use of something as potentially harmful as radiation to kill cancer often results in uncertainty and fear among both actual and potential patients. Several myths have developed as a result. Here’s the truth behind these myths.
Will my hair fall out?
Hair loss is normally caused by chemotherapy drugs that move throughout the body, effectively poisoning the entire system. Radiotherapy is a ’local’ treatment, using beams directly focused on the targeted area so hair loss is unlikely except in areas where the beam is targeted at your head.
Does it hurt?
Most radiotherapy patients say they feel nothing other than a slight tingling during delivery. Over time, the skin in the area being treated may become dry, sore or itchy, but usually the discomfort is tolerable. With newer, more targeted forms of radiotherapy, this kind of side effect is minimized.
Does it burn the skin?
There’s a possibility of very slight sun burning, but nothing unduly uncomfortable.
Are there really unpleasant side effects?
Very few, thanks to more focused and precise treatment techniques. Radiotherapy can cause harm if critical organs, glands and tissue are overly exposed, which is why modern treatments intend to minimize contact with them. Debilitating side effects are far more common with chemotherapy.
Will I have to stay in hospital?
Unlike surgery, radiotherapy is non-invasive and doesn’t require a stay in hospital. It’s an outpatient treatment.
Will it make you radioactive?
No. The high energy x-rays used in external beam radiotherapy treatments switch on and off like a light-bulb. There is no residual radiation when the beam is turned off.
About Varian Medical Systems
Varian Medical Systems is the worlds leading manufacturer of medical devices and software for treating cancer and other medical conditions with radiotherapy, radiosurgery, proton therapy, and brachytherapy. The company supplies informatics software for managing comprehensive cancer clinics, radiotherapy centers and medical oncology practices. Varian is a premier supplier of tubes and digital detectors for X-ray imaging in medical, scientific, and industrial applications and also supplies X-ray imaging products for cargo screening and industrial inspection.
Varian supplies close to two out of every three external beam radiotherapy machines installed globally. More than 5,500 Varian medical linear accelerators for cancer radiotherapy and radiosurgery are in service around the world, treating tens of thousands of patients per day. The company also produces advanced brachytherapy and proton therapy systems for treating cancer.
Varian X-ray tubes are sold to most major diagnostic equipment manufacturers and cover a range of applications including advanced mammography and CT scanning. The company also produces real-time, digital X-ray image detectors, which are incorporated in many types of diagnostic imaging systems. Away from medical, the companys Security and Inspection group is the market leader in high-energy X-ray devices for non-destructive testing and cargo screening.
Varian’s global headquarters is in Palo Alto, California, and the company’s largest European manufacturing site is in Crawley, England. Varian employs nearly 5,000 people at manufacturing sites in North America, China, and Europe and in 60 sales and support offices around the world.
Varian has a long history of pioneering in the world of radiotherapy. The company was founded (as Varian Associates) in the late 1940s by a group of scientists with strong connections to Stanford University. The company’s founders included brothers Russell and Sigurd Varian, inventors of the klystron tube, a high-frequency amplifier for generating microwaves that became an essential component of the modern medical linear accelerator. During the 1950s and 1960s, Varian Associates invented or commercialized many technologies, including X-ray tubes and linear accelerators. In the late 1960s, the company developed the medical linear accelerator for radiation therapy. Ultimately, linear accelerators displaced cobalt as the radiation therapy method of choice. In early 1999, Varian Associates changed its name to Varian Medical Systems after spinning off its semiconductor manufacturing equipment business and its scientific instruments business. Today Varian Medical Systems is the world’s leading supplier.